Along with the physical changes that occur as we get older, there are changes to our sleep patterns.
As people age they tend to have a harder time falling asleep and more trouble staying asleep than when they were younger.
It is a common misconception that sleep needs decline with age. In fact, research demonstrates that our sleep needs remain constant throughout adulthood.
Why do older people have problems?
Changes in the patterns of our sleep – what specialists call “sleep architecture” – occur as we age and this may contribute to sleep problems. Sleep occurs in multiple stages including dreamless periods of light and deep sleep, and occasional periods of active dreaming (REM sleep). The sleep cycle is repeated several times during the night and although total sleep time tends to remain constant, older people spend more time in the lighter stages of sleep than in deep sleep.
Many older adults also report feeling more tired during the day. Studies on the sleep habits of older people show an increase in the time it takes to fall asleep, an overall decline in REM sleep, and an increase in sleep fragmentation (waking up during the night) with age.
The reported prevalence of sleep disorders also tends to increase with age. However, research suggests that much of the sleep disturbance among the elderly can be attributed to physical and psychiatric illnesses and the medications used to treat them.
In addition to changes in sleep architecture that occur as we age, other factors affecting sleep are the circadian rhythms that coordinate the timing of our bodily functions, including sleep e.g older people tend to become sleepier in the early evening and wake earlier in the morning compared to younger adults.
This pattern is called advanced sleep phase syndrome. The sleep rhythm is shifted forward so that 7 or 8 hours of sleep are still obtained but the individuals will wake up extremely early because they have gone to sleep quite early. The reason for these changes in sleep and circadian rhythms as we age is not clearly understood. Many researchers believe it may have to do with light exposure and treatment options for advanced sleep phase syndrome typically include bright light therapy.
The prevalence of insomnia is also higher among older adults and up to 44% experience insomnia on some nights of the week or it can become chronic.
People with insomnia can experience excessive daytime sleepiness, difficulty concentrating, and increased risk for accidents and illness as well as significantly reduced quality of life so it should be taken seriously.
It is worth speaking to your doctor or pharmacist about insomnia symptoms and about any effects these symptoms may have. Your doctor can help assess how serious a problem it is and what to do about it. The doctor can review your medications to see if you are taking anything that is increasing the problem.
They can discuss any other medical problems that might be causing the inability to sleep.
You may receive a prescription for sleeping tablets as a short term solution or try some of the very good over the counter remedies such as Nytol. Take it around 30 mins before going to sleep. You can take this with other tablets such as paracetamol. Check with your GP if you are on other medications.
Nytol Original and Nytol One-A-Night contain a commonly used antihistamine called diphenhydramine hydrochloride. It works by blocking the normal actions of histamine, the chemical that stimulates arousal-promoting areas of the brain. This helps reduce alertness and promote that first drowsy stage of sleep, helping you to drift off into a restful, deeper sleep
There are some other simple things to try
1. Limit your caffeine intake
Caffeine has a half life of 6 hours and a quarter life of 12hours which means if you drink a coffee at midday 25% of the caffeine is still working at midnight


2. Limit screen time such as computers, phones and ipads, at least one hour before bedtime. Blue light stops the body producing melatonin, which is what helps you to go to sleep.
3. Sleep in the darkness– darkness causes the body to release melatonin a hormone that helps us sleep. Take away any clocks that have lights on.


4. Get 2-3 hours of sunlight a day– Just as darkness is important so is light which helps regulate the sleep cycle and melatonin levels.
5. Limit alcohol as this will cause you to wake up during the night while your liver works to break it down. This causes a rise in body temperature and can wake you up

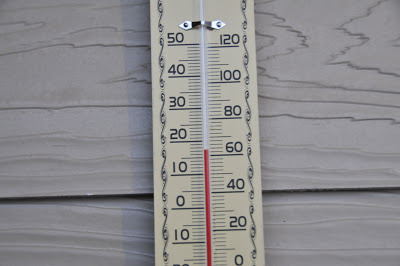
6. Keep the bedroom cool– Drop your core temperature at night by opening the window or setting the thermostat for around 17 degrees
7. Try and stick to a sleep schedule by going to bed and getting up at regular times. Try not to lie in bed awake for too long in the mornings or your brain does not associate bed with sleep


8. Try and keep your weight down as this increases the chance of snoring and sleep Apnoea
9. Do not eat too late so that the food is digested before you lie down.


10. Avoid drinking too much liquid 1 hour or so before bed– Although you need to remain hydrated avoid drinking too much water before bed so you are less likely to need the bathroom in the night.
11. Try listening to the radio or a talking book in order to nod off
12. Aim to get 8 hours of sleep
Studies now indicate that a lack of sleep can increase the chance of diabetes, obesity and Alzeimer’s
A lack of sleep leaves a high level of cortisol ( stress hormone) in the body.
13. Ty and take regular exercise of some sort each day- Even if you have mobility problems try and find some aerobic activity that you can do such as walking or swimming. Even some exercises in your chair could help


Aerobic exercise helps older adults sleep better
A study at Northwestern University found that aerobic exercise resulted in the most dramatic improvement in quality of sleep, including sleep duration, for middle-aged and older adults with a diagnosis of insomnia.
- The participants exercised for two 20-minute sessions or one 30-to-40-minute session four times per week.
- They worked at 75 percent of their maximum heart rate on at least two activities including walking or using a stationary bicycle or treadmill.
- Their sleep quality improved from a diagnosis of poor sleeper to good sleeper.
- They reported fewer depressive symptoms, more vitality, and less daytime sleepiness.
Source: National Sleep Foundation
14. Social interaction is also helpful
Try going to a club or exercise class, or consider joining a voluntary organisation to help
Getting back to sleep at night
As you get older, it is normal to wake up more often during the night.
If you are having trouble falling back asleep try these these things
1. Do not stress!! Stressing over the fact that you can not get back to sleep only encourages your body to stay awake.
2. Try to relax rather than sleep- Try a relaxation technique such as deep breathing or meditation, without getting out of bed.
To do this take a deep breath and then release it very slowly.
This helps lower your heart rate and can be very effective in helping you relax and go back to sleep.
3. Do a quiet, non-stimulating activity. If you’ve been awake for more than 20 minutes, get out of bed and do a non-stimulating activity, such as reading a book. But keep the lights dim and avoid screens.
4. Write down anything you are worrying about – then look at it next morning.
You will find it is not as bad in the light of day!


Should I avoid an afternoon nap?
A new study suggests that a siesta or afternoon nap is very effective in lowering blood pressure.
It also has a beneficial effect on any disc problems in the back. When you lie down your discs expand again and relieve any pressure that might be causing nerve pain or sciatica.
If you do take a nap make sure it is early in the afternoon so it will not interfere with your bedtime.
Try and limit it to 15-45 mins. It would be safer to set an alarm so you do not sleep too long.
Power naps have been used very successfully by many including Winston Churchill who swore by his 20 minutes of ‘ blessed oblivion’ every afternoon.

Sleep Apnea
Loud snoring is particularly serious as it can be a symptom of obstructive sleep apnea (OSA) and is associated with high blood pressure and other health problems. With OSA, breathing stops – sometimes for as long as 10-60 seconds – and the amount of oxygen in the blood drops, often to very low. This alerts the brain, causing a brief arousal (awakening) and breathing resumes. These stoppages of breathing can occur repeatedly, causing multiple sleep disruptions throughout the night and result in excessive daytime sleepiness and impaired daytime function.
Untreated sleep apnea puts a person at risk for cardiovascular disease, headaches, memory loss and depression. It is a serious disorder that is easily treated.
If you experience snoring on a regular basis and it can be heard from another room or you have been told you stop breathing or make loud or gasping noises during your sleep, these are signs that you might have sleep apnea and it should be discussed with your doctor.
There is a simple machine that you can use at night,which controls this.

Restless legs syndrome (RLS)
This is a neurological movement disorders characterised by an irresistible urge to move the limbs. With RLS, unpleasant, tingling, creeping or pulling feelings occur mostly in the legs, becomes worse in the evening and make it difficult to sleep through the night. Its prevalence increases with age and about 10% of people in North America and Europe are reported to experience RLS symptoms. About 80% of people with RLS also have periodic limb movement disorder (PLMD) and in one study, it was found that approximately 45% of all older persons have at least a mild form of PLMD.
Although this is difficult to cure try exercise and stretches.
As we age, there is an increased incidence of medical problems, which are often chronic. In general, people with poor health or chronic medical conditions have more sleep problems e.g hypertension is associated with both snoring and OSA and heart failure is also linked with OSA.
Extracts from helpguide.com
National sleep foundation

