Although shoulder joint replacement is less common than knee or hip replacement, it is just as successful in relieving joint pain.
Shoulder replacement surgery was first performed in the United States in the 1950s to treat severe shoulder fractures.
Over the years, shoulder joint replacement has come to be used for many other painful conditions of the shoulder, such as different forms of arthritis.
There are now around 5000 replacements done a year and it is the third most common joint replacement operation.
If nonsurgical treatments like medications and activity changes are no longer helpful for relieving pain, you may want to consider shoulder joint replacement surgery. It is a safe and effective procedure which relieves your pain and helps you resume all your everyday activities.
The average age for people having a shoulder replacement is around 70 years old, with many people being well over 70. A modern artificial shoulder joint will usually last for at least 15-20 years so revision surgery is very rarely needed.
Anatomy
Your shoulder is made up of three bones: your upper arm bone (humerus), your shoulder blade (scapula), and your collarbone (clavicle). The shoulder is a ball-and-socket joint: The ball, or head, of your upper arm bone fits into a shallow socket in your shoulder blade. This socket is called the glenoid.

The surfaces of the bones where they touch are covered with articular cartilage, a smooth substance that protects the bones and enables them to move easily. A thin, smooth tissue called synovial membrane covers all remaining surfaces inside the shoulder joint. In a healthy shoulder, this membrane makes a small amount of fluid that lubricates the cartilage and eliminates almost any friction in your shoulder. The muscles and tendons that surround the shoulder provide stability and support.
All of these structures allow the shoulder to rotate through a greater range of motion than any other joint in the body.
Causes of shoulder problems which might lead to the need for replacement
Osteoarthritis (Degenerative Joint Disease)
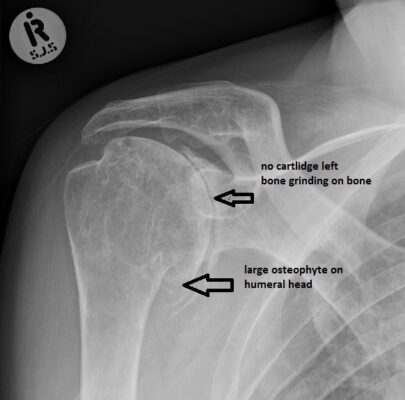
This is an age-related “wear and tear” type of arthritis. It usually occurs in people 50 years of age and older, but may occur in younger people, too. The cartilage that cushions the bones of the shoulder softens and wears away. The bones then rub bone on bone which gradually leads to shoulder stiffness and painful.
Unfortunately, there is no way to prevent the development of osteoarthritis and is a common reason people have shoulder replacement surgery.
Rheumatoid Arthritis
This is a disease in which the synovial membrane that surrounds the joint becomes inflamed and thickened. This chronic inflammation can damage the cartilage and eventually cause cartilage loss, pain, and stiffness in multiple joints including the shoulder.
Post-traumatic Arthritis
This can follow a serious shoulder injury. Fractures of the bones or tears of the tendons or ligaments around the shoulder may damage the articular cartilage over time. This leads to shoulder pain and limits function.
Rotator Cuff Tear Arthropathy
A patient with a large, long-standing rotator cuff tear may develop cuff tear arthropathy. This in turn leads to arthritic changes in the articular surface of the shoulder joint
Avascular Necrosis (Osteonecrosis)
Avascular necrosis is a painful condition that occurs when the blood supply to the bone is disrupted for whatever reason. This leads to destruction of the shoulder joint and arthritis.
The risk factors that increase the chance of avascular necrosis are –
Chronic steroid use
Deep sea diving
Severe fracture of the shoulder
Sickle cell disease
Heavy alcohol use
Severe Fractures
A severe fracture of the shoulder is another common reason people have shoulder replacements. When the head of the upper arm bone has a complicated fracture it may be very difficult for a surgeon to put the pieces of bone back in place and the blood supply can be disrupted. In many cases a surgeon may recommend a shoulder replacement. This is especially common in older patients with osteoporosis as they are most at risk for severe shoulder fractures.

Is Shoulder Joint Replacement for You?
The decision to have shoulder replacement surgery should be one that is discussed between yourself, your GP, and the orthopaedic surgeon.
There are several reasons why your doctor may recommend shoulder replacement surgery.
People who benefit from surgery often have:
- Severe shoulder pain that interferes with everyday activities, such as reaching into a cupboard, dressing, toileting, and washing.
- Moderate to severe pain while resting. This pain may be severe enough to prevent sleeping normally
- Loss of motion and/or weakness in the shoulder.
- Failure to improve with other treatments such as anti-inflammatory medications, cortisone injections, and physiotherapy.
Orthopaedic Assessment
Your GP may refer you to an orthopaedic surgeon for a thorough evaluation to work out if you are a good candidate for this type of surgery.
The assessment with the orthopaedic surgeon will consist of several components:
- A full medical history including your general health. You will be asked about the extent of your shoulder pain and how it affects your day to day function.
- A physical examination which will see how much range of motion you have, the stability and strength.
- X-rays-These images will show the extent of damage to your shoulder including the amount of loss of the normal joint space between bones, irregularity in the shape of the bone, bone spurs, and loose pieces of cartilage or bone that may be floating inside the joint.
- Other tests to see the condition of the bone and soft tissues of your shoulder may include-
- Blood tests
- MRI scan
- Bone scan
The results of this will be discussed with you as to whether shoulder joint replacement is the best option to relieve your pain and improve your function.
Other treatment options — including medications, injections, physiotherapy, or other types of surgery — will also be discussed and considered.

Shoulder Replacement Options
Shoulder replacement surgery is highly technical. It should be performed by a surgical team with experience in this procedure.
There are different types of shoulder replacements and the surgeon will discuss with you which type of replacement would best suit you and why that choice is right for you.
Total Shoulder Replacement
The typical total shoulder replacement involves replacing the arthritic joint surfaces with a highly polished metal ball attached to a stem and a plastic socket.
These components come in a variety of sizes and can be either cemented or “press fit” into the bone. If the bone is of good quality, your surgeon may choose to use a non-cemented (press-fit) humeral component. If the bone is soft, the humeral component may be implanted with bone cement. In most cases an all-plastic glenoid (socket) component is attached with bone cement.
Implantation of a glenoid component is not advised if:
- The glenoid has good cartilage
- The glenoid bone is severely deficient
- The rotator cuff tendons are irreparably torn
Patients with bone-on-bone osteoarthritis and intact rotator cuff tendons are generally good candidates for conventional total shoulder replacement.

Stemmed Hemiarthroplasty
Depending on the condition of your shoulder, your surgeon may replace only the ball. This procedure is called a hemiarthroplasty (half a replacement!)
In a traditional hemiarthroplasty, the head of the humerus is replaced with a metal ball and stem, similar to the component used in a total shoulder replacement. This is called a stemmed hemiarthroplasty.
Some surgeons recommend hemiarthroplasty when the humeral head is severely fractured but the socket is normal.
Other indications for a hemiarthroplasty include:
- Arthritis that only involves the head of the humerus with a glenoid that has a healthy and intact cartilage surface
- Shoulders with severely weakened bone in the glenoid
- Some shoulders with severely torn rotator cuff tendons and arthritis
Sometimes the decision between a total shoulder replacement and a hemiarthroplasty, has to be taken in the operating room at the time of the surgery.
Studies show that patients with osteoarthritis get better pain relief from total shoulder arthroplasty than from hemiarthroplasty.
Resurfacing Hemiarthroplasty
Resurfacing hemiarthroplasty involves replacing just the joint surface of the humeral head with a cap-like prosthesis without a stem. With its bone preserving advantage, it offers those with arthritis of the shoulder an alternative to the standard stemmed shoulder replacement.
This may be an option for you if:
- The glenoid still has an intact cartilage surface
- There has been no fresh fracture of the humeral neck or head
- There is a desire to preserve humeral bone
For patients who are young or very active, resurfacing hemiarthroplasty avoids the risks of component wear and loosening that may occur with conventional total shoulder replacements in this patient population. It is also easier to convert to total shoulder replacement if necessary at a later date.
Reverse Total Shoulder Replacement
Another type of shoulder replacement is called reverse total shoulder replacement.
Reverse total shoulder replacement is used for people who have:
- Completely torn rotator cuff muscles with severe arm weakness
- The effects of severe arthritis and rotator cuff tearing (cuff tear arthropathy)
- Had a previous shoulder replacement that failed.
In these cases a normal total shoulder replacement may still leave them with pain and unable to lift their arm up past 90-degrees which may be very debilitating.
In this procedure the socket and metal ball are switched around so that a metal ball is attached to the shoulder bone and a plastic socket is attached to the upper arm bone. This allows the patient to use the deltoid muscle instead of the torn rotator cuff to lift the arm. It sounds odd but is very effective.

Complications of Shoulder Replacement surgery
Your surgeon will explain all the potential risks and complications of shoulder joint replacement surgery.
Most complications are successfully treatable. Possible complications include the following.
Infection
Infection is a complication of any surgery. In shoulder joint replacement, infection may occur in the wound or deep around the prosthesis. It may happen while in the hospital or after you go home or even years later. Minor infections in the wound area are generally treated with antibiotics. Major or deep infections may require more surgery and removal of the prosthesis.
Any infection in your body can spread to your joint replacement.
Prosthesis Problems
Although prosthesis designs and materials, as well as surgical techniques, continue to advance, the prosthesis may wear down and the components may loosen. The components of a shoulder replacement may also dislocate. Excessive wear, loosening, or dislocation may require revision surgery.
Nerve Injury
Very rarely nerves in the vicinity of the joint replacement may be damaged during surgery. These nerve injuries usually improve with time and may completely recover.
Preparing for Surgery
If you decide to go ahead with shoulder replacement surgery your orthopaedic surgeon may ask you to schedule a have a full physical examination with your GP before surgery to make sure you are healthy enough for the surgery. Many patients with chronic medical conditions such as heart disease may also be required to see a specialist, such a cardiologist, before the surgery.
Medications
You will be asked what medications you currently take. Some medications may need to be stopped before surgery e.g the following over-the-counter medicines may cause excessive bleeding and should be stopped 2 weeks before surgery:
- Non-steroidal anti-inflammatory medications, such as aspirin, ibuprofen, and naproxen sodium
- Most arthritis medications
If you take blood thinners, either GP or cardiologist will advise you about stopping these medications before surgery.

Planning your return home
If you take time to make some simple changes at home before surgery it will make your recovery period easier.
For the first few weeks following surgery it will be hard to reach high shelves and cupboards so before your surgery go through your home and put things you may need afterwards on lower shelves.
When you come home from the hospital you will need help for a few weeks with some daily tasks such as dressing, bathing, cooking and cleaning. If you do not have any help at home you may need to book a short stay in a rehabilitation home. Another option is to book some form of carer either live in or part time.

The Surgery
Before the Operation
Wear loose-fitting clothes and a button-front shirt when you go to the hospital for your surgery. After the surgery you will be wearing a sling and will have limited use of your arm.
Your anaesthesist will discuss with both you and your surgeon the type of anaesthestic to be used. The options are-
1. General anaesthetic where you are asleep for the whole operation
2. Local anaesthetic where you are awake but have no feeling around the surgical area
3. Often a combination of both types are used such as a general with an Interscalene Block ( a form of local) which gives you a pain-free arm for 20 hours or so after surgery. This means you wake up pain free.
Surgical Procedure
The procedure to replace your shoulder joint with an artificial device usually takes about 1 ½ to 2 hours.
The surgery involves making an incision at the front of the shoulder. The head of the humerus and glenoid are replaced with artificial components to replace the worn cartilage. Often cement and/or screws are used to hold the components in place.
After surgery, you will be moved to the recovery room where you will remain for several hours while your recovery from the anaesthetic is monitored. Then you will be taken back to your room.
Recovery
Your medical team will give you several doses of antibiotics to prevent infection. Most patients are able to eat solid food and get out of bed the day after surgery. You will most likely be able to go home on the first, second or third day after surgery.
Pain Management
Following the surgery your arm will feel numb because of the nerve block/local anaesthetic used during your operation but this should wear off during the first twenty four hours. Post-operative pain is normal and you will receive a combination of painkillers to help minimise this pain. It may take several months for the pain to fully settle but long-term your level of pain should be significantly reduced from before your operation
Pain is a natural part of the healing process. Your doctor and nurses will work to reduce your pain, which can help you recover from surgery faster.
Medications are often prescribed for short-term pain relief after surgery. Many types of medicines are available to help manage pain including opioids, non-steroidal anti-inflammatory drugs (NSAIDs) and local anaesthetics. Your doctor may use a combination of these drugs to relieve your pain and minimise the need for opioids.
Opioids are very helpful to relieve pain after surgery but are very addictive. Opioid dependency and overdose has become a serious problem so it is very important to use them as directed by your doctor. As soon as your pain improves it is best to stop taking opioids and move on to other forms of painkillers.
After the operation
Sling-you will be put in a sling both for comfort and to protect the shoulder. You can take it on and off as you wish and you do not need to have your arm strapped to your body. The physiotherapists and nurses will show you how to take the sling on and off. You will gradually wear the sling less over the next 4–8 weeks.
Sleeping-You may find it helpful to wear the sling at night particularly if you tend to lie on your side. Or you can use pillows in front of you to rest your arm on. If you are lying on your back to sleep you may find placing a thin pillow or folded towel under your upper arm will be more comfortable.
Ice
Icing the shoulder may help to reduce any pain and minimise any swelling. We would advise you to wrap a bag of frozen peas in a damp tea towel and apply directly to your shoulder. You can do this for 10 to 15 minutes each time three times a day or more if required.
Pain management is an important part of your recovery. Talk to your doctor if postoperative pain becomes a problem.
Rehabilitation
A careful, well-planned rehabilitation program is critical to the success of a shoulder replacement. You usually start gentle physiotherapy soon after the operation. Your surgeon or physiotherapist will provide you with a home exercise program to strengthen your shoulder and improve flexibility.
Your Recovery At Home
When you leave the hospital your arm will be in a sling. You will need the sling to support and protect your shoulder for the first 2 to 4 weeks after surgery.
Wound care
You will have staples running along your wound or a suture beneath your skin. The staples will be removed several weeks after the surgery but the suture below the skin will not require removal.
Avoid soaking the wound in water until it has thoroughly sealed and dried. You may continue to bandage the wound to prevent irritation from clothing.
How do I know if there is a problem?
Please contact your GP if you experience any of the following:
-Increasing pain
-Increasing redness
-Swelling or oozing around the wound site
-Fever (temperature higher than 37.5°C)
-Sudden inability to move your arm.
Activity
Exercise is a critical component of home care, especially during the first few weeks after surgery. Follow the home exercise plan that you have been given to help you regain your range of motion and strength.
Most patients are able to perform simple activities such as eating, dressing and washing within 2 weeks after surgery. Some pain with activity and at night is common for several weeks after surgery.
Driving a car is not allowed for 2 to 4 weeks after surgery.
Do’s and Don’ts
The success of your surgery will depend largely on how well you follow your orthopaedic surgeon’s instructions at home during the first few weeks after surgery. Here are some common do’s and don’ts for when you return home:
- Don’t use the arm to push yourself up in bed or from a chair because this requires forceful contraction of muscles.
- Do follow the program of home exercises prescribed for you. You may need to do the exercises 2 to 3 times a day for a month or more.
- Do not overdo it! Even if your shoulder pain has now been eased by the surgery do not be lulled into thinking that you can do more than is prescribed. Early overuse of the shoulder may result in severe limitations in motion.
- Do not lift anything heavier than a glass of water for the first 2 to 4 weeks after surgery.
- Do plan assistance at home if you do not have anyone there.
- Do not participate in contact sports or do any repetitive heavy lifting after your shoulder replacement.
- Do avoid placing your arm in to any extreme positions, such as straight out to the side or behind your body for the first 6 weeks after surgery.
Rehabilitation
Phase 1.
Immediately after the operation until you are discharged You will start to move the shoulder with the help of the physiotherapist, but to begin with you will be quite one-handed. If your dominant hand (right hand if you are right-handed) is the side with the operation, your daily activities will be affected and you will need some help. Activities that are affected include dressing, bathing, hair care, shopping and preparing meals.
The occupational therapist will discuss ways and show you how to be as independent as possible during this time.
Before you are discharged from hospital, the staff will help you plan for how you will manage when you leave. Please discuss any concerns with them.
Phase 2
After you have been discharged and for up to 6 weeks after the operation the pain in your shoulder will gradually begin to reduce . Wean yourself out of the sling slowly over this time, using it only when you feel necessary. Do not be frightened to try and use your arm at waist level for light tasks. You will be seeing a physiotherapist and doing regular exercises at home to get the joint moving and to start regaining muscle control. If you feel unsure about what you can or cannot do, please discuss this with the physiotherapist. Lifting your arm in front of you may well still be difficult at this stage.
Phase 3
6-12 weeks
The pain should be gradually resolving. The exercises are now designed to improve the movement available and get the muscles to work, taking your arm up in the air or away from your body when you are sitting or standing. You will have an increasing ability to use your arm for daily tasks.
Phase 4
After 12 weeks
You can progress to more vigorous stretches if this is necessary for the activities that you want to do. You can now work on gradually regaining your full muscle strength. which may take up to a year. Occasionally the muscles are badly damaged which prevents you regaining full strength despite your best efforts. Even in these cases the pain in the shoulder joint will still be much less than before your operation and often you can find small ‘trick’ movements that enable you to do what you want to do. Most improvement will be felt in the first 6 months, but strength and movement can continue to improve for 18 months to 2 years.
Guide to daily activities in the first few weeks
Some difficulties are quite common, particularly in the early stages so you will need some help over the first few weeks.
The occupational therapist (O.T.) will help you to be as independent as possible during your rehabilitation. Special equipment can be borrowed from the O.T. department if needed and any problems can be discussed with them.
Getting on and off seats- If you were having problems getting up from chairs, beds or the toilet before the operation it will be harder after the operation. You may need a seat raise such as an extra cushion or blocks to put under the chair and bed.
Getting in and out of the bath- Ideally the first few days you should strip wash or shower. If you do not have a shower you may need a bath board to help you get in to the bath and you can wash there. You may also need long handled brushes and sponges.
Hair care –You may need to get help with this or go to a local hairdresser
Dressing– Initially it will be difficult to dress and to put under garments on alone. It is best to wear loose clothing, either with front fastening or ones which you can slip over your head.
When you are dressing put the operated arm in first and do the reverse when you undress i.e your operated arm last.
There are other aids available to you such as dressing sticks, shoe horns and elastic shoe laces.
Eating- Use your operated arm to eat when you feel able
Returning to work
You will probably be off work approximately 6–8 weeks, depending on the type of job you have.
If your job requires lifting, overhead activities or heavy manual work you are advised not to do these for 3 to 6 months.
Return to sports and hobbies
This will depend on the level of your pain, range of movement and the strength that you have regained in your shoulder following the operation.
Start with short sessions, involving little effort and gradually increase e.g
- Swimming – after 6 weeks
- Gardening light tasks such as weeding but no heavy jobs or digging– after 6–8 weeks
- Bowls – after 3–6 months
- Golf, tennis, badminton or squash – after 4–6 months

Here is the link to the list of exercises.
Driving
You cannot drive while in a sling – even if you have an automatic – because your insurance company will not cover you. This means you cannot drive for at least 6 weeks and it is normally about 8 weeks before you can drive comfortably. Try first doing a short drive around the block to make sure you feel safe.
Prognosis/ Outcome
You should be much improved by 3 months. You should have active movement above 90 degrees so be able to get your hand comfortably to your head and maybe a bit above and be functioning rather well in front of you. So day-to-day activities should be fine.
By 6 months you should be very good with the range of movement nearly the same as your good side and the strength coming back. At this point you should be returning to your usual activities and sports.
The best results are in older patients who had surgery for osteoarthritis, as they give the joints less stress. Younger patients tend to fare worse and may develop loosening of the joint.
Interesting facts
- One study found that of patients who underwent hemiarthroplasty, 82% were still functional after 10 years and 75% after 20 years. For total shoulder arthroplasty the figures were 97% at 10 years and 84% at 20 years.
- Outcome is best for an experienced surgeon who performs high volumes of shoulder arthroplasty or hemiarthroplasty operations.
- Pre-operative planning, attention to anatomy, and an optimum rehabilitation programme are the keys to success.
- Improvement in function can continue for up to 18 months after the operation