What is sciatica?
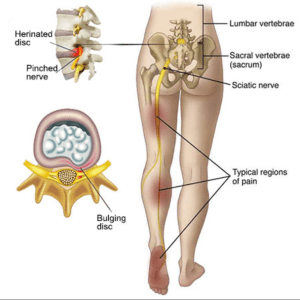
Sciatica is the term used for anyone with pain that radiates down some or all of the distribution of the sciatic nerve. Some experts estimate that up to 40 per cent of people will experience sciatica at least once in their life. Anything that irritates this nerve can cause pain, ranging from mild to severe.
Sciatica is usually caused by a compressed nerve in the lower spine.
The sciatic nerve is the longest and widest nerve in the human body running from the lower few vertebrae of the back through the buttocks and down the back of the leg.
The Sciatic nerve controls several muscles in the lower leg and supplies sensation to the skin of the foot and most of the lower leg.
What is the cause?
A variety of lower back conditions may lead to sciatica.
Causes of Sciatica
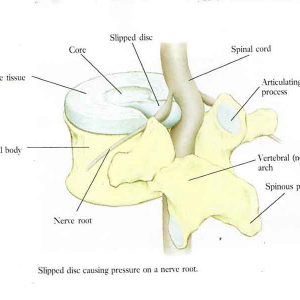
1. Degenerative disc disease (disc protrusion or large tear in the disc)
2. Muscle spasm in the back or buttocks.
3. Arthritis of the spine and the formation of osteophytes
4. Lumbar spinal stenosis (narrowing of the spinal canal in the lower back)
5. Spondylolisthesis (a condition of the spine where one vertebra slips forward on another one)
6. Pregnancy
What are the symptoms?
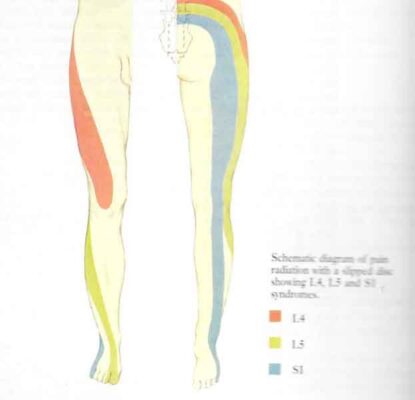
1. Low back pain
2. Pain in the buttock and /or down the leg generally worse on sitting
3. Pain around the hip area
4. Burning and tingling down the leg
5. Sharp shooting pains down the leg
6. Sometimes weakness and numbness. If this is causing difficulty lifting the foot seek immediate consultation with a doctor
7. Pain is normally relieved by lying down
8. Pain is made worse by certain movements such as bending forwards
Prognosis and Treatment
In most cases, sciatica will resolve within 6 weeks and with the help and advice of a physiotherapist this can often be speeded up. Once the pain of sciatica passes, there are strengthening and postural exercises, stretches and other measures that help prevent its return.
How is Sciatica Diagnosed?
Sciatica is a clinical diagnosis based on your symptom description, the behaviour of your pain and a thorough physical examination.
While the diagnosis of sciatica is reasonably simple, the cause of your sciatica may require further investigations to eliminate or confirm its origin. It is also important to determine how significant your sciatic nerve has been compressed. The physiotherapist will be able to determine how serious it is and whether urgent investigation is needed.
The role of the physiotherapist-
Your physiotherapist will examine you, paying special attention to your spine and legs. In addition to asking you if you have low back pain that spreads to the leg and calf, your physiotherapist will test you for muscle weakness, sensation deficits and altered reflexes in your leg or foot.
They will also want to ask you about your general health such as any injury, a recent fever, any problems controlling your bowels or bladder, any previous cancers, weight loss or gain, any osteoporosis, tablets you are taking and any other relevant conditions you have had. The answers to all these questions build up a full picture and will alert the therapist to any more serious causes of the sciatica such as a bone fracture, infection or cancer.
Your physiotherapist or doctor may send you for X-rays or arrange for a CT scan or an MRI scan to ascertain the cause of the pressure on the nerve. Most cases of sciatica affect the L5 or S1 nerve roots.
The physiotherapist will also advise you about how to sit, how to relieve the pressure on the nerve such as heel raises in your shoes and walking with short strides. You may also be taught some simple stretches and exercises and advised about pain relief.
Advice to aid Pain relief
Heat and Ice- Simple use of Ice packs or Hot baths
Painkillers- Pain relievers such as Paracetamol and Neurofen taken at regular intervals- These can be spread out so you take each of them 4 hourly but you can take paracetamol then 2 hours later Neurofen then 2 hours later the paracetamol etc. This keeps a level of pain relief in the blood all the time. This in turn means you will be able to move more freely.
Avoid sitting for long or at all if this increases your pain. Some people find sitting on a wedge helps a lot which alters the angle of your back and puts less pressure on the spine. The good old fashioned kneeling chair is also very useful if you need to be able to sit.
Lie down- Have periods of lying down during the day if you can. Just 30 mins in the middle of the day can allow the spinal discs to re-expand and ease the pressure on the nerve to allow you to continue the rest of your day with less pain
Walk with shorter strides
Wear shoes with rubber soles or preferably an Air Nike type of trainer. A heel pad can also help such as a silicon heel cup.
Muscle relaxants-Sometimes muscle relaxants (such as diazepam) can help but will only be prescribed for a few days.
Other drugs-Anti-inflammatories and anti-depressants are sometimes prescribed. Anti-depressants may seem a strange way to treat sciatica but they can help by reducing pain perception in the brain. Sometimes, when none of these drugs work, then you may be prescribed such as gabapentin and duloxetine.
Gabapentin is an anti-epileptic drug or anticonvulsant. It primarily affects chemicals and nerves in the body that are involved in the cause of seizures and some types of pain. It has been found to help nerve related type of pain.
Epidural injection- If none of the above is controlling the pain, you will be offered an X ray guided epidural injection into the spine. This is a very safe procedure and Cortisone will be injected into the correct area of the spine to help settle the pain and inflammation. It is especially useful for the referred leg pain. It can take 2-7 days to work so be patient and has a 50-90% chance of success. You can have up to 3 injections 1 month minimum apart over one year.

Physiotherapy treatment
Most sciatic pain is treated and managed with conservative treatment.
As sciatica can be caused by a range of different issues as described above, it is important that an appropriate assessment is performed to provide specific treatment. Not all sciatic pain is the same!
It is quite common for the lower back to be the source of the sciatic leg pain, but the person will often not feel any pain in the lower back.
Treatment with your physiotherapist should include
- Advice and education about the condition and how to manage the symptoms, generally exercise and staying active rather than bed rest
- Strengthening exercises for supporting muscles e.g. lower back, core, hip
- Stretching exercises for tight muscles
- Hands on treatment for stiff joints and/or tight muscles
- An individualised exercises program for self-management and future prevention.
Most cases of sciatica resolve by themselves within six weeks to three months and are not serious. The next step would be an ultrasound guided injection. If this does not work then rarely, a surgical technique known as micro-discectomy is required, to remove a small piece of disc that has fully compressed the nerve.
The main treatment focus needs to be on the person and their symptoms and goals, and not the image findings. The scan results are only a piece of the diagnostic puzzle, not the absolute answer. Many people with terrible x-rays and scans recover without surgery.
For lists of possible exercises and stretches see the end of this article
Surgery
If none of the above work, then you may need surgery. This surgery is a minimally invasive procedure performed on patients with a herniated lumbar disc. During this surgery the surgeon removes portions of the herniated disc to relieve pressure on the spinal nerves.
The advantages of surgery are that there can be up to an 80-90% chance of significant relief of leg pain. However there is no guarantee that there will be any relief from back pain or an improvement in any leg weakness or changes in sensation/feeling that you may have had prior to surgery
The risks of the surgery
These are all rare and increasingly rare with all the up to date surgical advances.
1. The usual risks from the anaesthetic.
2. A small risk of increased pain in back or leg
3. Risk of injury to the nerves causing weakness or numbness in the legs and / or the genital or anal area.
4. Risk of injury to the nerves that supply the bladder, bowel and sex organs, which could result in problems with bladder, bowel and sexual function
5. Leak of spinal fluid
6. Infection, this includes infection from MRSA bacteria (infection with MRSA is rare).
7. Haematoma, (blood clot) In 6% of patients another piece of disc at the same level can move out and cause pressure again.
It is also possible for a prolapsed (slipped) disc to occur at another level in the spinal column at some time in the future.

Prevention of sciatica
In many cases sciatica can be prevented by good posture, regular exercise, building up core strength and being very careful when lifting heavy objects. Be aware that lifting and twisting whilst holding a heavy item can cause microtrauma to the discs.
Over your life you will undoubtedly have a few micro-tears. It is particularly important to be careful as you get older as these microtears can more easily develop into a full-blown disc protrusion.
When to seek urgent help
Pain from sciatica results from damage to the patient’s nerve tissue. In the vast majority of cases, the nerve damage is not permanent. However, the following signs indicate that there may be a more serious problem that requires immediate medical attention:
- Patients who feel weakness or numbness may require surgery, and any patient experiencing these symptoms should seek professional attention.
- Patients who experience bowel or bladder incontinence (inability to control the bowel or bladder) and/or increasing weakness or loss of sensation in the legs should see a doctor immediately.
Some simple exercises and stretches you can do at home can help ease pain from sciatica (pain in your buttocks, legs and feet) and improve your strength and flexibility.
Aim to do these exercises every day, along with other activities like walking, swimming or yoga.
Your pain should start to ease within 2 weeks and will usually pass in about 4 to 6 weeks.
Knee hugs
Lie on your back and pull one knee into your chest.
Then release.
Repeat x 5

Sciatic mobilising stretch
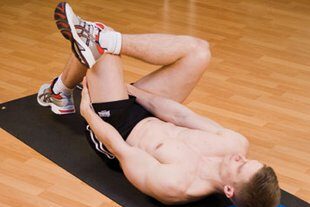
Start position: Lie on your back. Place a small, flat cushion or book under your head. Bend your knees and keep your feet straight and hip-width apart. Keep your upper body relaxed and your chin gently tucked in.
Action: Bend one knee up towards your chest. Hold the back of your upper leg with both hands, then slowly straighten the knee. Hold for 20 to 30 seconds, taking deep breaths. Bend the knee and return to the starting position.
Repeat 2 or 3 times, alternating legs.
Tips:
- Don’t press your lower back down into the floor as you stretch.
- Only stretch as far as is comfortable. See below



Back extension
Lie on your front and rest on your forearms with your elbows bent at your sides. Look towards the floor and keep your neck straight.
Keeping your neck straight, arch your back up by pushing down on your hands. You should feel a gentle stretch in the stomach muscles. Breathe and hold for 5 to 10 seconds. Return to the starting position.
Repeat x 10
Standing hamstring stretch
Stand upright and raise one leg on to a stable object, such as a step. Keep that leg straight and your toes pointing up.
Lean forward while keeping your back straight. Hold for 20 to 30 seconds while taking deep breaths.
Repeat 2 or 3 times

Lying deep gluteal stretch
Lie on your back. Place a small, flat cushion or book under your head. Bend your left leg and rest your right foot on your left thigh.
Grasp your left thigh and pull it towards you. Keep the base of your spine on the floor throughout and your hips straight. You should feel the stretch in your right buttock. Hold for 20 to 30 seconds while taking deep breaths.
Repeat x 3 times
Use a towel around your thigh if you can’t hold it.
Slump stretch in sitting
Sit in a chair and slouch your back keeping your head up to start with.
Then slowly lift your lower leg by straightening your knee.
Just go to the edge of the pain and only repeat x 5 times.
If you do not feel the stretch progress to doing the exercise with your head flexed forwards which adds stretch into the spinal tissues.


Gluteal stretch in sitting
Another type of gluteal stretch can be done in sitting by placing the bad leg over the good one and then pull up the thigh with your hands x 2-3 holding for a few seconds.
Important exercises to do
General back mobilising exercises are worth doing to ease up any stiffness in the spine-
See program here
Back exercises- Basic mobilising
There are a variety of exercises in the water that are also very useful. See Hydrotherapy for the Back and sciatica here.
Sciatic nerve swing video clip-
Exercise sheet for the back in water-

