What is Osteoarthritis?
It is the most common form of arthritis with about 9 million people in the UK seeking treatment for it.
It is not to be confused with Rheumatoid arthritis. This type of arthritis is basically wear and tear and not a systemic disease like Rheumatoid.
When is it likely to get it?
Osteoarthritis is also most commonly seen in people middle-aged to elderly and is the top cause of disability in those age groups, although it can also appear in younger people who have sustained joint injuries.

What happens to the joint in Osteoarthritis?
All articular surfaces of the joints in the body are covered with cartilage which has no blood supply and therefore does not heal well when injured. The function of this cartilage is to reduce friction between the surfaces of the bones. All the nutrients needed for the cartilage is supplied by the synovial fluid which is secreted by the membrane lining the joint capsule.
The term osteoarthritis predominately means degeneration and excessive wear of the articular cartilages (wear and tear) and also involves some changes to the underlying bone.
The condition is one which develops and advances with increasing age. It can be primary or secondary.
Primary occurs more often in women and diabetics. Obesity may not necessarily the cause of early onset of OA but does accelerate the process once it has begun.
Secondary OA follows an injury or joint disease. This may be after fractures involving the joint, repetitive overloading of joints, ligament injuries, dislocations, infections and rheumatoid arthritis.
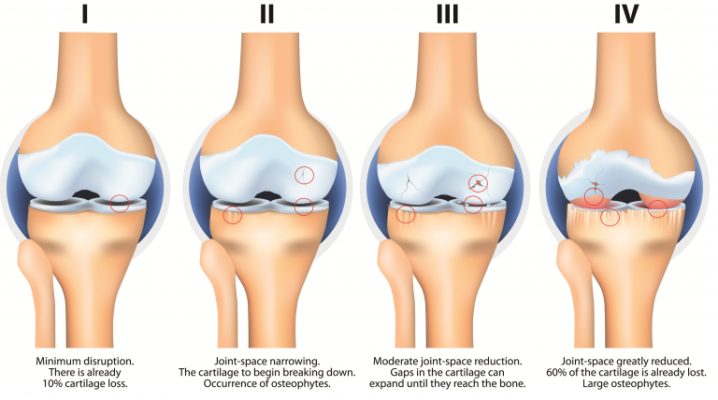
Whatever the cause the changes to the joint are the same. Initially the cartilage softens, then the surface becomes uneven and small cracks appear which may extend down into the bone. Eventually the cartilage is worn away to reveal the bone and the joints become bone on bone. The bone surface hardens which is called sclerosis.
- Extra bone may form at the edge of the joint forming bony growths called osteophytes and these can sometimes restrict movement or rub against other tissues. In some joints, eg the finger joints, these may be seen as firm, knobbly swellings over the joints.
- The lining of the joint capsule (called the synovium) may thicken and produce more fluid than normal, causing the joint to swell.
- Tissues that surround the joint and help to support it may stretch so that after a time the joint becomes less stable. Many joints also lose muscle strength if there is persistent swelling in the joint.
Which joints are most commonly affected?
The joints most often affected by arthritis are Hip, Knee, Shoulder, Spine, Hands and Feet.
Causes are generally-
- Old age
- Genetic recurrence or defect
- Overuse of joints
- Job stresses
- Sports injuries or previous injuries involving the joints
- Obesity increases speed of degeneration
What are the symptoms and diagnosis of OA
- Pain – usually present may be just after certain activities but as it progresses it can become a feature at rest and disturb your sleep
- Morning stiffness or stiff after a prolonged period of rest
- Joint abnormalities- these may include swelling, loss of range of motion, atrophy of the muscles, tenderness, increased temperature of the joint, instability of the joint and grinding noises(crepitus) during movement
- Xrays changes- will show narrowing of the joint space, cysts, osteophytes and sclerosis
While rheumatoid arthritis occurs symmetrically in the body i.e when a joint on one side is affected, the joint on the other side will likely be affected as well—
Osteoarthritis does not occur symmetrically in the body. It affects a single joint or a joint on one side of the body more severely.
Treatment for Osteoarthritis
Like Rheumatoid arthritis and other similar diseases of the joints, damage from OA cannot be reversed. However, there are treatment options and lifestyle changes that can reduce pain and improve the function and delay further degeneration.
1. Lose weight
Being overweight is a large risk factor for osteoarthritis because it puts a large amount of stress on weight-bearing joints.
Every pound of excess weight exerts about 4 pounds of extra pressure on the knees. So a person who is 10 pounds overweight has 40 pounds of extra pressure on his knees; if a person is 100 pounds overweight, that is 400 pounds of extra pressure on his knees.
This chart shows the different amount of stress on the joints during a variety of exercises.
If you are carrying extra weight all of these figures will be increased substantially.
Activities of daily living
Activity | Peak Tibial Forces (×BW) | Notes |
2.5 – 2.8 | Laboratory floor | |
Treadmill Walking [51] | 2.1 ± 0.2 | 1 to 3 miles per hour |
Power walking [51] | 2.8 ± 0.4 | 4 miles per hour on treadmill |
Jogging [46] | 3.1 – 3.6 | Tumor replacement prosthesis |
Jogging [51] | 4.2 ± 0.2 | 5 miles per hour on treadmill |
Stationary Bicycling [51] | 1.0 – 1.5 | Level 1–5; 60–90 rpm |
Golf (lead knee) [51] | 4.4 ± 0.1 | Left knee in a right handed golfer |
Golf (trailing knee) [51] | 3.0 ± 0.2 | |
Tennis serve [51] | 4.2 ± 0.1 | |
Tennis forehand [51] | 4.3 ± 0.4 | |
Tennis backhand [51] | 3.5 ± 0.6 | |
StairMaster Level 1 [51] | 2.4 ± 0.1 | |
StairMaster Level 3[51] | 3.3 ± 0.3 | |
Elliptical Level 1[51] | 2.3 ± 0.2 | |
Elliptical Level 11[51] | 2.2 ± 0.3 | |
Leg Press [51] | 2.8 ± 0.1 | Foot reaction force = 1 ×BW |
Knee Extension [51] | 1.5 ± 0.0 | Resistance = 0.2 ×BW |
Rowing machine [51] | 0.9 ± 0.1 |
Overall stationary bicycling generated even lower knee forces than walking.
Tennis, also considered a high-impact activity, generated high knee forces in the same range as treadmill jogging.
The golf swing, although considered a low impact activity, generated high peak tibial forces in the leading knee approaching those of jogging.
Elliptical trainers, a low-impact exercise machine, are often recommended for patients who experience knee pain during higher impact jogging. Elliptical training generated forces comparable to treadmill walking.
Rowing machines, often recommended to increase knee flexion, generated low forces. Both the leg press (against a resistance force equal to body weight) and the squat generated the same peak tibial forces. The leg-press machine can therefore be recommended to build up to a squat, if a full weight-bearing squat is not possible.


Exercise
It is important to keep as much as range of motion as possible and strengthen all the supporting muscles in a way that does not aggravate the symptoms.
For example the knee tends to lose the ability to fully straighten which in turn seriously affects the way the knee functions. It is very important to try and keep full extension of the knee. There are exercises described in the knee exercises section showing you how to do this.
However you may want to initially consult a physiotherapist who will prescribe the correct programme for you. They will also analyse your gait to see whether you need orthotics and any walking aid.
Hydrotherapy exercises are an excellent option as this avoids straining the joints by weight bearing.
See Hydrotherapy section on this site
Hydrotherapy/ Exercises in water
See Exercise section on this site
Home remedies
There are all sorts of ideas of what might help. Many sufferers have found significant pain and inflammation relief and sometimes complete remission with lab grade turmeric and boswellia combinations. These seem to be especially effective when combined with an autoimmune diet.


Medications
Osteoarthritis is treated with many of the same medications as rheumatoid arthritis.
Nonsteroidal anti-inflammatory drugs (NSAIDs) to decrease swelling and pain are often the first method of treatments.
Other options include topical drugs such as anti-inflammatory gels bought over the counter which can be applied directly to the skin..
Corticosteroids given as an injection into the joint are often used to provide temporary relief of OA and can delay the need for surgery. They can also provide a pain free window to help working on the physiotherapy.
Ultimately when the pain becomes unbearable surgery is an option. These will be discussed under each part of the body.
The degree of damage to a joint is not very helpful in predicting how much pain you will have. Some people have a lot of pain and mobility problems from a small amount of damage to the joint, while others have a lot of damage to the joint but few or no symptoms.
So although Xray is a useful tool do not be put off by the Xray findings!
References Sports Injuries Dr Lars Peterson and Dr Peter Renstrom
NCBI article Knee joint forces: prediction, measurement, and significance

