Are you short of breath or is it Just old age?
How age affects the Respiratory System
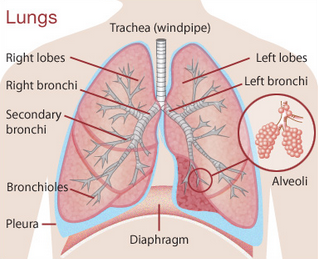
The respiratory system consists of a group of organs that work together to take in oxygen and get rid of carbon dioxide as you breathe. When you breathe in the oxygen-rich air goes down the main bronchus then into smaller tubes called bronchioles. Finally, at the end of the bronchioles are small, round air sacs called alveoli These sacs are surrounded by tiny blood vessels (capillaries). When air enters the alveoli, oxygen moves through to the capillaries and thereby enters the bloodstream. Likewise, carbon dioxide moves from the capillaries into the alveoli sacs and enables the body to expel it by breathing out.
Like all things that change with age the respiratory system is not immune to changes which gradually decline over time. Like other muscles in your body, the muscles that enable your breathing become weaker, which in turn means that you inhale and exhale less air and breathing becomes shallower. This can also be affected by pain and illness. The lungs also become less elastic as you get older which means they do not expand and contract as well. On top of this certain changes occur in the nervous system that make coughing less effective which in turn can lead to a less productive cough and a build up of mucus in the lungs.
All of these changes can lead to an increased susceptibility to infections, such as pneumonia and the flu.
In healthy people, these age-related changes rarely lead to symptoms. Importantly, age-related changes in the lungs compound the effects of heart and lung diseases, especially those caused by the destructive effects of smoking.
Other causes of Shortness of Breath
if you are bothered by constant coughing and wheezing, you may have something called chronic obstructive pulmonary disease (COPD).
Approximately 1.2 million people have been diagnosed with chronic obstructive pulmonary disease (COPD) in the UK while eight million have asthma.
COPD is a group of progressive lung diseases which includes emphysema and chronic bronchitis. These are usually the result of smoking or exposure to air pollution or chemical fumes.
People with COPD have persistent shortness of breath which can disrupt the way you lead your everyday life.
Reasons for COPD
- Loss of elasticity of the lung tissue and air sacs
- The walls between the air sacs are damaged.
- The walls of the airways thicken and become swollen.
- The airways make more mucus than normal which can clog airways.
Common symptoms of COPD include:
- a persistent cough that produces a lot of mucus
- shortness of breath felt especially on exertion or during exercise
- a wheeze while breathing
- a feeling of tightness in the chest
All these symptoms are not a natural part of aging.
So, if you do experience these symptoms it is best to contact your doctor.
Early treatment can help slow the progress of the condition and help improve your quality of life.
Very important if you have the following symptoms go STRAIGHT to Accident and Emergency:
- difficulty talking or breathing
- blue or grey fingernails or lips
- lack of mental alertness
- very fast heartbeat
Diagnosing COPD
The GP will ask about the history of your symptoms and examine your chest. They may also request a chest X-ray or CT scan of your lungs which will may show signs of COPD and is useful to help rule out any other possible causes.
Usually your doctor will use a spirometry test to diagnose COPD which involves you exhaling into a machine which measures how quickly you can exhale air out of your lungs and the quantity of air expelled. Generally, this figure is less anyway when you age but those with COPD that figure is much reduced.

Treatment for COPD
Once you have the correct diagnosis your doctor will prescribe you medications to help with your breathing such as Inhaled short and long-acting bronchodilators (puffers) and corticosteroids.
Use of inhalers
The NICE guidelines for adults with COPD (2018) say patients should only be prescribed an inhaler after being shown how to use it, and if their clinician is confident that they can use it correctly. Inhaler technique should also be regularly assessed, particularly if their condition is not under control and whenever they change devices, medication or doses.
see Asthma UK for a video to show you how to use it correctly.
Your doctor may also recommend that you make certain lifestyle adjustments such as:
- giving up smoking
- eating a healthy diet with plenty of vegetables and fruit
- taking vitamin and mineral supplements if needed
- start taking exercise at least three times per week
In severe cases of COPD oxygen therapy may be needed.
Extracts from
Asthma UK. How to use your inhaler. London: Asthma UK; 2018.
NICE. Chronic obstructive pulmonary disease in over 16s: diagnosis and management. NG115. London: National Institute for Health and Care Excellence; 2018.


